Sodium balance and its disorders
Sodium (Na) is the primary electrolyte that regulates extracellular fluid levels in the body. The mineral is thus essential for tissue hydration because it moves from the cell interior to the extracellular space and in turn pumps water into the cell.[i]
Therefore, extracellular Na concentrations are much higher (140 mmol/L) than those in the intracellular space (10 mmol/L). Based on this innate property, Na is involved in the regulation of blood volume, blood pressure, transport of numerous nutrients and cellular waste products, tissue growth, bone mineralization, neurotransmission and multiple other functions. Consequently, it is highly conceivable that these Na-associated functions may be affected by any disorder that leads to acute or chronic imbalances of Na homeostasis.
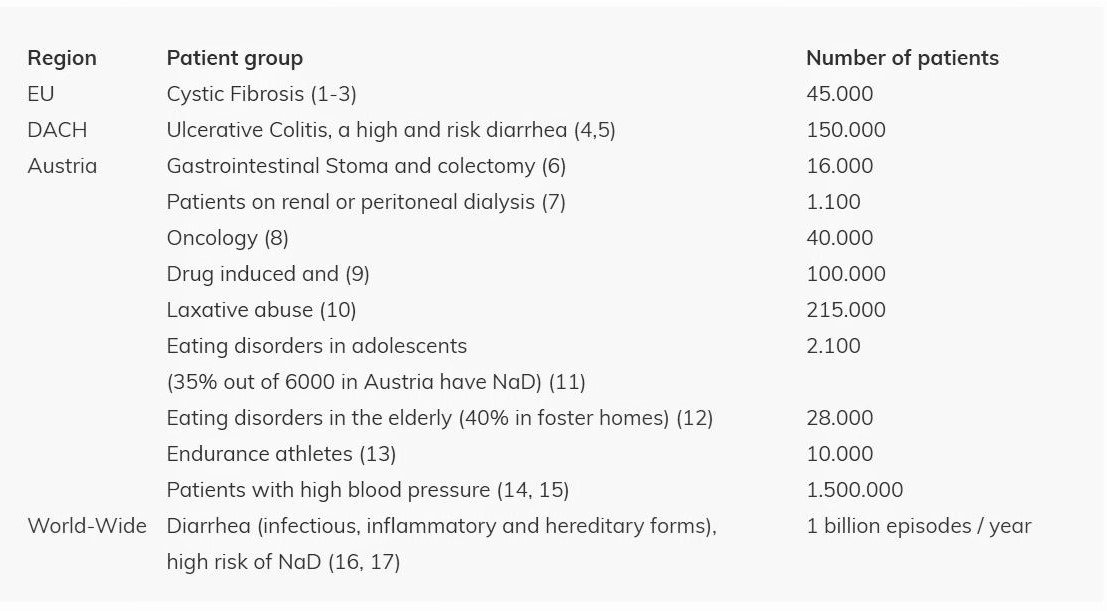
Disorders causing Na depletion (NaD) or Na overload (NaO) in the human body are significant health issues affecting approximately two billion people worldwide.
NaD is an often underestimated and neglected disorder that results from an imbalance of fluid and Na in the human body. The pathological decrease of total body Na is the result of an increased loss of Na, as may occur in patients with diarrhea,[ii], [iii], [iv], [v] gastrointestinal stoma,[vi] cystic fibrosis,[vii], [viii] hemodialysis[ix] or during phases of intense physical exercise with enhanced sweating. [x] Furthermore, NaD may also be a result of low Na intake in the case of malnutrition, as for example in patients with anorexia nervosa.[xi] NaD may cause common nonspecific symptoms such as sleeping disorders,[xii] fatigue, headache, confusion, low appetite[xiii] or growth failure,[xiv] but may also lead to severe complications such as muscle cramps, epilepsy, encephalopathy, coma and even death.
In the current clinical routine, the diagnosis of NaD is frequently missed because, in particular when occurring in its “hidden” form as the so-called normonatremic Na depletion (NNaD), it cannot be determined by the conventionally used method of measuring Na concentration in blood plasma.[xv] This parameter does only reflect the Na content in the circulating blood and not necessarily the amount of Na present in other compartments of the body such as the intracellular and interstitial spaces. Thus, when patients suffer from proportionate losses of Na and fluid, the blood Na concentration remains normal, even if a NaD-causing disorder is present. This often happens in patients having chronic diarrhea,[iv] gastrointestinal stoma [vi] and cystic fibrosis.[vii], [viii]
Na overload (NaO), on the other hand, results mainly from increased salt intake and has become a food industry-borne epidemic worldwide.[xvi] It mainly occurs due to inappropriate “salting” in industrialized food production and is well known to patients and doctors as an important cause of arterial hypertension and its sequelae such as cardiac insufficiency and stroke. According to a recent published analysis of the NCD Risk Factor Collaboration, alone in Austria, 1.5 million people are estimated to be affected by high blood pressure diseases and would benefit immensely from a simple tool to control their body sodium status for better management of their dietary salt intake.[xvii]
Na-PoCT market potential focused
“only” on patients with high medical need
[i] Lang F, Persson PB, Murer H. Regulation des inneren Milieus. In:
Schmidt RF, Lang F, Heckmann M. In:Physiologie des Menschen. 31. Auflage. Heidelberg: Springer, 2010. S. 630-6932
[ii] Okposio MM, Onyiriuka AN, Abhulimhen-Iyoha BI. Point-of-admission serum electrolyte profileof children less than five years old with dehydration due to acute diarrhea. Trop Med Health43:247-52(2015)3
[iii] Heinz-Erian P, Akdar Z, Haerter B, Waldegger S, Giner T, Scholl-Bürgi S, Müller T. Urinaryexcretion markers identify sodium depletion in pediatric acute gastroenteritis. Klin Pädiatr228:24-8(2016)
[iv] Heinz-Erian P, Müller T, Krabichler B, Schranz M, Becker C, Rüschendorf F, Nürnberg P, RossierB, Vujic M, Booth IW, Holmberg C, Wijmenga C, Grigelioniene GG, Kneepkens CMF, Rosipal S, Mistrik M, Kappler M, Michaud L, Dozcy LC, Siu VM, Krantz M, Uterman G, Janecke AR. Mutationsin SPINT2 cause a syndromic form of congenital sodium diarrhea. Am J Hum Genet 84:188-96(2009)
[v] Bilal A, Sadig MA, Haider N. Frequency of decreased hyponatremia and hypokalemia inmalnourished children with acute diarrhea. J Pak Med Assoc 66:1077-80(2016)
[vi] Bower TR, Pringle KC, Soper RT. Sodium deficit causing decreased weight gain and metabolicacidosis in infants with ileostomy. J Pediatr 23:567-72(1988)
[vii] Knepper C, Ellemunter H, Eder J, Niedermayr K, Haerter B, Hofer P, Scholl-Bürgi S, Müller T,Janecke AR, Heinz Erian P. Low sodium status in cystic fibrosis – as assessed by calculatingfractional Na+-excretion – is associated with decreased growth parameters. J Cyst Fibr 14:400-405(2016)
[viii] Coates AJ, Crofton PM, Marshal T. Evaluation of salt supplementation in CF infants. J Cyst Fibr8:382-5(2009)
[ix] Dekker MJ, Marcelli D, Carnaud B, Konings CJ, Leunissen KM, Levin NW, Carioni P, Maheshwari V, Raimann JG,van der Sande FM, Usvyat LA, Kotanko P, Kooman JP. Unraveling the relationship between mortality,hyponatremia, inflammation and malnutrition in hemodialysis patients: results from the international MONDOinitiative. Eur J Clin Nutr 70:779-84(2016)
[x] Mayer CU, Treff G, Fenske WK, Blouin K, Steinaker JM, Allolio B. High incidence of hyponatremia in rowersduring a four-week training camp. Am J Med 128;1144-51(2015)
[xi] Levy-Shraga Y, David D, Vered I, Kochavi B, Stein D, Modan-Moses D. Hyponatremia and decreased bonedensity in adolescent inpatients diagnosed with anorexia nervosa. Nutrition 32:1097-1102(2016)
[xii] Rodriguez MJ, Alcaraz A, Solana MJ, Garcia A. Neurological symptoms in hospitalizedpatients: do we assess hyponatremia with sufficient care? Acta Paediatr 103: e7-e10(2014)
[xiii] Corona G, Guiliani C, Parenti G, Parenti G, Norello D, Verbalis JG, Forti G, Maggi M, Peri A. Moderatehyponatremia is associated with increased risk of mortality: evidence from a meta-analysis. PLOS ONE8:e80451(2013)
[xiv] Wassner SJ, Kulin HE. Diminished linear growth associated with chronic salt depletion. Clin Pediatr29:719-21(1990)
[xv] Thomas L. Messung von Natrium. In: Labor und Diagnose.TH-Books 5th edition, Chapter 8.2, pp 295-303.
[xvi] Subasinghe AK, Arabshani S, Businye D, Evans RG, Walker KZ, Ridell MA, Thrift AG. Association between salt and hypertension in rural and urban populations of low and middle income countries: a systematic review and metaanalysis of population-based studies. Asia Pac J Clin Nutr 25:402-13(2016)
[xvii] http://www.statistik.gv.at/web_de/statistiken/index.html
1) ECFSPR Annual Report 2016, Orenti A, Zolin A, Naehrlich L, van Rens J et al, 2018.
2) Mirtajani SB, Farnia P, Hassanzad M, Ghanavi J, Farnia P, Velayati AA. Geographical distribution of cystic fibrosis; The past 70 years of data analyzis. Biomed Biotechnol Res J 1:105-12(2017)
3) Burgel P.R et al. Future trends in cystic fibrosis demography in 34 European countries. Eur Respir J. 46(1):133-41(2015).
4) https://www.dccv.de; http://www.efcca.org/
5) Burish J. et al. The burden of inflammatory bowel disease in Europe. J Crohn’s Col. 7:322-337(2013)
6) Heikens JT, de Vries J, van Laarhoven CJ. Quality of life, health-related quality of life and health status in patients having proctocolectomy with ileal pouch-anal anastomosis for ulcerative colitis: a systematic review. Colorectal Dis 14:536-44(2012)
7) Dekker MJ, Marcelli D, Carnaud B, Konings CJ, Leunissen KM, Levin NW, Carioni P, Maheshwari V, Raimann JG, van der Sande FM, Usvyat LA, Kotanko P, Kooman JP. Unraveling the relationship between mortality, hyponatremia, inflammation and malnutrition in hemodialysis patients: results from the international MONDO initiative. Eur J Clin Nutr 70:779-84(2016)
8) Hackl M, Karim-Kos HE. Krebserkrankungen in Österreich. Krebspublikation_2016
9) Liamis G, Milionis H, Elisaf M. A review of drug-induced hyponatremia. Am J Kidney Dis 52:144-53(2008)
10) Konsensuspapier Expertenforum: Obstipation und Laxanzien. In: Praxis. 88, 1269–1274(1999)
11) Levy-Shraga Y, David D, Vered I, Kochavi B, Stein D, Modan-Moses D. Hyponatremia and decreased bone density in adolescent inpatients diagnosed with anorexia nervosa. Nutrition 32:1097-1102(2016)
12) Kaeley N, Akram M, Ahmad S, Bhatt N. Hyponatremia in elderly – its prevalence, aetiology and outcome. Ann Internat Med Dent Res 3:16-19(2017)
13) Mayer CU, Treff G, Fenske WK, Blouin K, Steinaker JM, Allolio B. High incidence of hyponatremia in rowers during a four-week training camp. Am J Med 128;1144-51(2015)
14) NCD Risk Factor Collaboration, Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants Lancet 389:37-55(2017)
15) Subasinghe AK, Arabshani S, Businye D, Evans RG, Walker KZ, Ridell MA, Thrift AG. Association between salt and hypertension in rural and urban populations of low and middle-income countries: a systematic review and metaanalysis of population-based studies. Asia Pac J Clin Nutr 25:402-13(2016)
16) http://www.who.int/en/news-room/fact-sheets/detail/diarrhoeal-disease
17) Janecke A, Heinz-Erian P, Müller T. Congenital sodium diarrhea: a form of intractable diarrhea with a link to inflammatory bowel disease. JPGN 63:170-6(2016)